In the realm of genetics and health, the study of epigenetics has emerged as a pivotal area of research with profound implications for understanding disease prevention and management. Epigenetics explores how external factors and lifestyle choices can influence gene expression without altering the underlying DNA sequence. This dynamic interplay between genes and environment highlights the potential for epigenetic mechanisms to play a critical role in disease susceptibility, progression, and prevention. This article delves into the fundamentals of epigenetics, its mechanisms, current research findings, and the implications for personalized medicine and public health strategies aimed at disease prevention.
Understanding Epigenetics
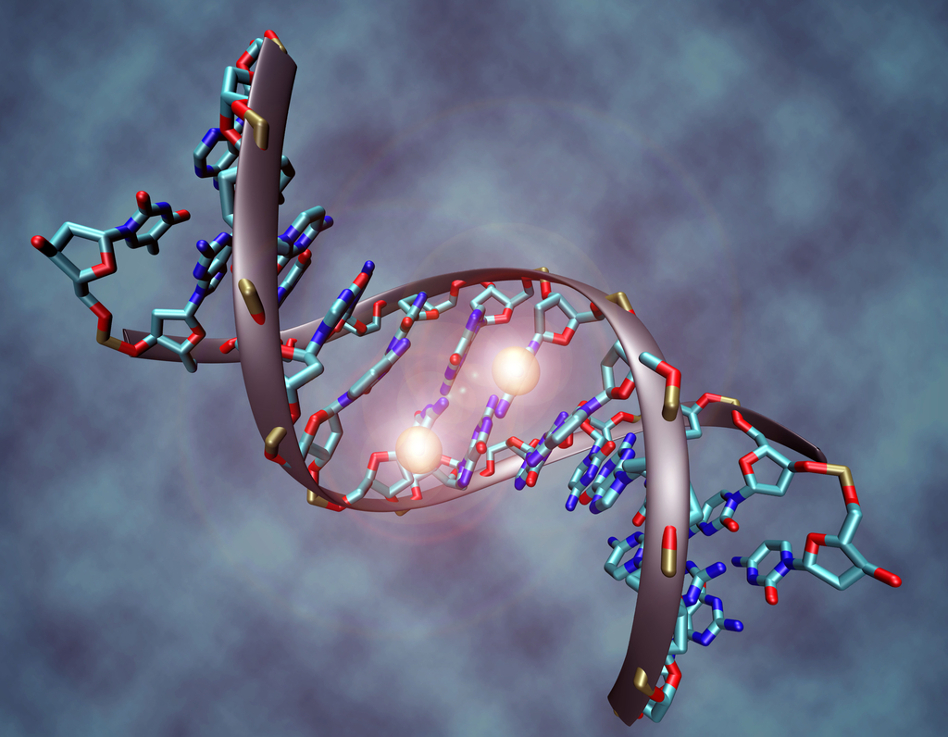
Epigenetics refers to changes in gene expression that occur without changes in the DNA sequence itself. While DNA provides the genetic blueprint for an organism, epigenetic modifications regulate which genes are turned on or off, influencing cellular function and behavior. These modifications include DNA methylation, histone modifications, and non-coding RNA molecules, all of which act as molecular switches to control gene activity.
DNA Methylation: Involves the addition of methyl groups to specific DNA sequences, typically resulting in gene silencing or reduced expression.
Histone Modifications: Alterations in the structure and function of histone proteins around which DNA is wrapped, influencing accessibility to genes for transcription.
Non-coding RNA: Regulates gene expression at the transcriptional or post-transcriptional level, affecting mRNA stability and protein synthesis.
These epigenetic changes can be influenced by a variety of factors, including diet, exercise, environmental exposures (such as pollutants and toxins), stress, aging, and even social interactions. Importantly, epigenetic modifications are reversible and can be responsive to interventions, making them promising targets for disease prevention and therapeutic strategies.
Epigenetics in Disease Prevention
The role of epigenetics in disease prevention is multifaceted, impacting a wide range of health conditions across the lifespan:
Cancer: Epigenetic alterations play a critical role in the development and progression of various cancers. DNA methylation patterns can serve as biomarkers for early detection and prognosis, while targeting epigenetic mechanisms with therapeutic agents holds promise for cancer treatment and prevention.
Cardiovascular Diseases: Epigenetic modifications contribute to the regulation of genes involved in lipid metabolism, inflammation, and vascular function. Lifestyle factors such as diet and exercise can influence these epigenetic changes, potentially mitigating cardiovascular risk.
Neurological Disorders: Epigenetic mechanisms are implicated in neurodevelopmental disorders, neurodegenerative diseases (such as Alzheimer’s and Parkinson’s), and mental health conditions. Understanding how environmental factors influence brain epigenetics could lead to preventive strategies and novel therapies.
Metabolic Disorders: Obesity, type 2 diabetes, and metabolic syndrome are influenced by epigenetic modifications that affect insulin sensitivity, adipocyte function, and energy metabolism. Lifestyle interventions, including dietary modifications and physical activity, can modify these epigenetic patterns and reduce disease risk.
Autoimmune Diseases: Epigenetic dysregulation contributes to aberrant immune responses seen in autoimmune conditions like rheumatoid arthritis, lupus, and multiple sclerosis. Identifying epigenetic signatures may aid in early diagnosis and development of targeted therapies.
Epigenetic Mechanisms and Environmental Factors
Environmental exposures can profoundly impact epigenetic mechanisms, potentially altering gene expression patterns across generations through a phenomenon known as transgenerational epigenetic inheritance. Studies have shown that factors such as prenatal nutrition, exposure to pollutants, stress, and lifestyle habits (smoking, alcohol consumption) can induce epigenetic changes that influence disease susceptibility in offspring.
Prenatal and Early Life Exposures: The fetal environment can shape epigenetic programming, affecting lifelong health outcomes. Maternal nutrition, stress levels, and exposures to environmental toxins during pregnancy can influence offspring’s susceptibility to chronic diseases later in life.
Nutrition and Diet: Dietary factors, including micronutrient intake (such as folate, vitamin B12, and methyl donors), bioactive compounds (like polyphenols), and dietary patterns (such as Mediterranean diet), can modulate epigenetic marks involved in disease prevention. For example, folate deficiency can lead to hypomethylation and increased cancer risk.
Physical Activity: Regular exercise has been shown to induce beneficial epigenetic changes associated with improved cardiovascular health, insulin sensitivity, and cognitive function. Exercise-mediated alterations in DNA methylation and histone modifications contribute to adaptive physiological responses.
Stress and Psychosocial Factors: Chronic stress can trigger epigenetic modifications that impact immune function, inflammation, and mental health. Mind-body interventions (such as meditation and mindfulness) may counteract stress-induced epigenetic changes, promoting resilience and well-being.
Implications for Personalized Medicine and Public Health
The field of epigenetics holds significant promise for advancing personalized medicine approaches and informing public health strategies aimed at disease prevention:
Precision Medicine: By integrating epigenetic data with genetic and clinical information, healthcare providers can tailor prevention and treatment strategies to individual patients’ epigenetic profiles. Personalized interventions based on epigenetic biomarkers may improve treatment outcomes and reduce adverse effects.
Early Detection and Screening: Epigenetic biomarkers have the potential to enhance early detection of diseases before clinical symptoms manifest, enabling timely interventions and preventive measures.
Lifestyle Interventions: Promoting healthy lifestyle behaviors, including balanced nutrition, regular physical activity, stress management, and avoidance of environmental toxins, can modify epigenetic patterns to reduce disease risk.
Policy and Environmental Regulations: Incorporating epigenetic research into public health policies may inform regulations on environmental exposures, occupational hazards, and consumer products to minimize adverse epigenetic effects and promote population health.
Challenges and Future Directions
Despite the promising potential of epigenetics in disease prevention, several challenges remain:
Complexity and Variability: Epigenetic regulation is complex and varies across individuals and tissues. Understanding the functional consequences of specific epigenetic changes and their interactions with genetic factors requires further research.
Ethical Considerations: Ethical issues related to privacy, consent, and the use of epigenetic data in healthcare must be addressed to ensure equitable access and protection of individuals’ rights.
Translation to Clinical Practice: Translating epigenetic research findings into clinical practice requires validation of biomarkers, development of standardized assays, and integration into healthcare systems.
Long-Term Effects and Intergenerational Implications: Investigating the long-term effects of epigenetic modifications and their potential transmission to future generations is crucial for understanding disease risk across the lifespan.
Conclusion
Epigenetics represents a paradigm shift in our understanding of gene-environment interactions and disease susceptibility. By elucidating how external factors influence gene expression and cellular function, epigenetics offers novel insights into disease prevention and personalized medicine strategies. Embracing epigenetic research holds the promise of promoting health, improving outcomes, and advancing equitable healthcare practices. As we continue to unravel the complexities of epigenetic regulation, integrating these insights into clinical care and public health initiatives will be essential for realizing the full potential of epigenetics in shaping a healthier future.